Politics in the Spotlights - Introduction November 2021 Report Indonesia Investments
In felt like a real déjà vu. Shortly before writing this introduction, the World Health Organization (WHO) said it added a new variant of concern to its list of COVID-19 mutations. This new variant, which is called Omicron (B.1.1.529), is believed to stem from South Africa or Botswana, and might be more contagious than the Delta variant that has been dominant over the past 12 months or so.
The claim that Omicron ‘might be highly infectious’ is based on the rapidly growing number of COVID-19 cases in South Africa. In October and the first half of November 2021, South Africa had very low numbers of COVID-19 cases. But then, there arrived a big and sudden burst of COVID-19 cases in the last week of November 2021 around Pretoria (one of South Africa’s three capital cities). When scientists investigated the cases it turned out to be this new Omicron variant.
When this news spread in late-November 2021 it immediately caused stocks and oil to drop sharply around the world. And, when it was confirmed that the new variant had spread to various continents, countries banned direct flights from South Africa, while Israel and Japan closed their borders to foreign travelers, and Great Britain and Australia tightened rules for all arrivals. Actually, this is where I experienced the real déjà vu. Some 20 months after ‘all hell broke loose’ when it was confirmed that COVID-19 was spreading around the world in Q1-2020, we now seem to be back where we started (if Omicron is indeed as infectious as media portray it to be; for now there exists no evidence as scientists have just started studying this variant).
These developments actually show to what extent the world has been affected in a psychological sense. Without actually waiting for some evidence of whether the new variant is indeed more infectious and/or more fatal, some far-reaching decisions are made and imposed (for example by closing borders and banning flights). Sure, it will be too late to take such actions once evidence is put on the table because the variant will have arrived by then (well, it will probably already be too late by the time the new variant is detected as these viruses spread very fast in today’s globalized world where people are very mobile). But, is going into a sort of lockdown when a variant of concern emerges really the more rational option?
We should also not forget that the median infection fatality rate (IFR) for COVID-19 is estimated at 0.23 percent based on a paper (titled Infection Fatality Rate of COVID-19 Inferred From Seroprevalence Data) that is available on the WHO website (and considering the actual total number of COVID-19 infections is likely higher than the number of confirmed infections, the median IFR could in fact be substantially lower than this 0.23 percent; something that is acknowledged on page 8 of this paper).

What the COVID-19 pandemic particularly exposes is the shortage of capacity in the healthcare systems around the world. In many nations capacity in hospitals has been cut hugely over the past couple of decades, while their populations grew rapidly and aged over the same time (implying there is a growing number of people with fragile immune systems and/or underlying illnesses, hence comorbidity has been the main complicating factor in terms of COVID-19 fatalities).[1] While 0.23 percent might seem a small figure (and, obviously, we have to multiply it by, well, perhaps five – if not much more – to include those people who require medical assistance but do survive the virus), it is a big group in absolute terms that certainly is way too big to handle in case they fall ill around the same time. So, indeed, measures are needed to limit the spread of COVID-19 in society (most notably through proper indoor ventilation, vaccines for the vulnerable, and by encouraging people to lead a healthy lifestyle).
But considering people will need to learn to live with COVID-19 in society as there are no signs that the virus will ever leave, it is of crucial importance to raise capacity in hospitals (or wider: in healthcare) in a structural manner. In developed nations healthcare systems have been made so efficient (through economization, meaning: saving money by spending less) that these systems collapse when a completely new and dangerous virus arrives (which, fortunately, is a rare phenomenon). Therefore, big public investment is needed in healthcare. If not, we can basically say “bye, bye” to economic and social growth as we knew it in the decades prior to the COVID-19 crisis as the costs of lockdowns are simply too high (such as children’s’ reduced long-term prospects because of the reduced quality of education, increase in depressions, cancelled/delayed treatment for other diseases, massive unproductive government spending and debt accumulation, mass unemployment, and loss of civil liberties).
However, the reason why it might be unlikely for governments to change course now (meaning reducing their focus on vaccines for whole populations, from young to old) is that this would imply acknowledging that their previous strategy was not the best one. The ‘point of no return’ seems to have been passed by early 2021.
Meanwhile, in response to the Omicron variant, Pfizer Inc. announced to deliver an updated COVID-19 vaccine in 100 days, while Moderna Inc. expects its own Omicron vaccine to be ready by early 2022. Again, a déjà vu. A year ago, these companies were racing to manufacture the first COVID-19 vaccine. But after expensive and intensive vaccination programs around the world, we are basically still in the same situation. Indeed, the number of COVID-19-related deaths has tumbled significantly in most countries compared to the first waves around Q2-2020 and Q3-2020. This could be the positive impact of the COVID-19 vaccines but, on the other hand, it could also be the case (like we see with the flu) that excess and under-mortality alternate (after a season of excess mortality there tends to be one or two seasons of under-mortality).

The underlying problem is that we still lack knowledge and therefore have to be very careful when making any firm conclusions. Another interesting dilemma is choosing between believing those who argue that unvaccinated people encourage mutations, or, those who argue that the vaccinated people encourage COVID-19 mutations (as vaccine-induced immunity could force the virus to mutate to survive). Well, the truth is probably a bit more complicated and somewhere in the middle. And there should actually be some considerable overlap between both categories considering many of the unvaccinated people have built immunity via natural infections (evidenced by antibodies found in unvaccinated blood donors), while part of the vaccinated people do get infected shortly after vaccination (and after some six months vaccine-induced protection against infection is almost gone completely). So, it is crucial to stay open- minded, factual and rational, both for policymakers and the people, in a world that is showing some very worrying polarization on all fronts. If not, it opens the doors to wrong, even fatal, decisions.
‘Indonesia Miracle’
Even without the arrival of a more contagious variant, various countries in Europe have, again, went into a sort of lockdown-mode as COVID-19 cases have been rising sharply across the region despite these countries having high vaccination rates.
And then, there is the ‘Indonesia miracle’. Since mid-July 2021 when only around six percent of the Indonesian population was fully vaccinated, there occurred a massive decline in new COVID-19 cases, up to the point where there are now only 200-400 new daily cases reported (out of a total population that numbers over 270 million people). It is a development we cannot attribute to the national vaccination program (although vaccines could certainly have contributed, albeit slightly, to the decline in cases over time).
And the same miracles occurred in countries like India and Japan. Strangely enough, though, we detect very little appetite from media or political leaders in the West to study the developments or government responses in these ‘miracle countries’, while – at least – some things must have gone right here (whether this was an intentional consequence of these countries’ policies or not –for example because herd immunity was perhaps largely achieved by the natural spread of the virus in society as people failed to comply with policies– comes second).
Is it these countries’ young age-structures that help explain these miracles? But, that would certainly not apply to Japan. Or, is it previous immunity from their exposure to other coronaviruses? Could it be lower infectious loads? Or, what I suspect, is it natural infection-induced immunity? Or, are there other, unknown, explanations? Is it a combination of factors? There could be very valuable lessons to be learned here for Western countries in their battle against COVID-19. However, for now, it seems that all that may undermine the existing strategy used in the West is simply ignored.
Daily New Confirmed COVID-19 Cases in Indonesia:
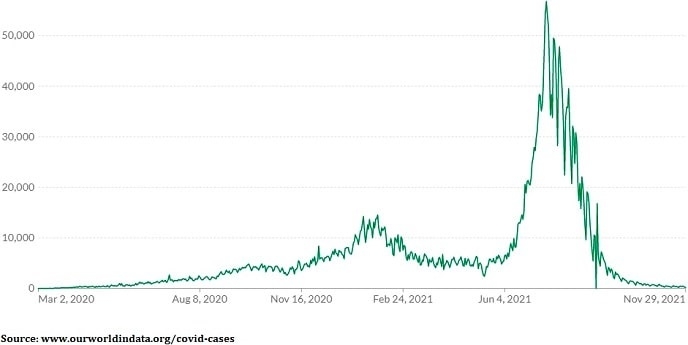
But although the COVID-19 referral hospitals are almost empty in Indonesia and few new COVID-19 cases are reported, we have to be careful. Since our knowledge of this virus (and why cases went down rapidly) is incomplete, it is certainly possible to see future COVID-19 waves. In fact, it is quite likely to see future waves as many experts agree that COVID-19 has become endemic (similar to the flu).
In fact, in mid-November 2021, local Indonesian news agency Kompas reported that the number of new COVID-19 cases and hospitalizations increased in 37 districts on Java and Bali. This could be related to the arrival of the rainy season (typically, the flu also peaks during the rainy season in Indonesia as people are more indoors, and perhaps lack sunlight, causing a shortage of vitamin D). In that context, it is also quite unfortunate that weather experts expect a very long rainy season due to the La Niña effect (which is the periodic cooling of ocean surface temperatures in the central and east-central equatorial Pacific that brings heavier tropical rainfall to Indonesia).
As a consequence, the Indonesian government remains cautious. Therefore, social and business restrictions will be turned up a notch, or two, (to PPKM Level 3) during the upcoming Christmas and New Year period across urban areas on Java and Bali. This is certainly not good for the economy. However, having in mind that the Delta variant spread rapidly shortly after the Idul Fitri (or Lebaran) holiday in May 2021, it might indeed be a good idea to limit traveling and the gathering of people for a day of ten (24 December 2021 – 2 January 2022). So, these days of stricter restrictions could indeed prevent bigger economic costs on the longer term.
To conclude on a positive note, if Omicron turns out to be more infectious, but less fatal (and this is a real possibility because – based on statements from virologists in global media – a virus that is more infectious tends to be less deadly, and vice versa), it could actually spread throughout the world making people immune (while causing limited numbers of casualties).
Next month, we should have more information on this topic. For now, we need to be cautious because Omicron is bound to spread everywhere. So, the best advice, in the meantime, is to eat healthy, exercise, take enough time to sleep at night, avoid stress, and get some sunshine in the morning (for vitamin D). This will do wonders for your immune system!
Richard van der Schaar
Managing Director
Indonesia Investments
Notes:
[1] While in many developed nations there occurred a significant reduction in capacity in hospitals over the past couple of decades, in emerging nations there exists structural undercapacity (due to weak healthcare systems). Both phenomena are causing great trouble in the COVID-19 crisis.
The November 2021 report can be ordered by sending an email to [email protected] or a message to +62.882.9875.1125 (including WhatsApp).
Price of this (electronic) report:
Rp 150,000
USD $10,-
EUR €10,-
Take a glance inside the report here!
.